COVID impacts medical research
Emergency state of health care leads to research breakthroughs
January 28, 2023
In January 2020, the World Health Organization declared COVID-19 as a global health emergency. The rapid spread of the disease immediately forced countries to implement public heath measures including lockdowns, quarantines, travel restrictions, and public closures, according to PubMed. With the development of this unknown, life-threatening disease, the public looked to scientists, specifically medical researchers for guidance on prevention and treatments, according to the National Academy of Medicine. According to The Lancet, this was the first time that scientists from around the world came together to combine resources and work on a specific disease, trying to discover the behavior of the virus and form treatments.
“As soon as SARS-CoV-2 was identified, scientists released the genetic code, so global scientists could begin working on vaccines,” said Dr. Eric Bing, Professor and Director at Southern Methodist University’s Center for Global Health Impact. “Free and abundant scientific collaboration happens when scientists are at our best, and this is exactly what happened in the early days of COVID-19.”
At the beginning of the pandemic, researchers began studying symptoms and risk factors of the disease. As COVID-19 progressed, researchers worked in public-private collaboration. Public-research universities worked with private bio-technology companies to find therapeutics and a vaccine. According to the NAM, the National Institute of Health, the source for the most biomedical research funding in the United States, worked with the government, companies and researchers to develop speed innovations through various technologies, supporting preventive treatment studies, and increasing the public’s knowledge about the disease. Most of this funding was given to researchers already working in epidemiology, leading scientists in other fields to experience a large decrease in resources, according to NAM.
“This collaboration was fueled by the fact that everyone was at risk with COVID-19, regardless of who you were and where you lived,” Dr. Bing said. “I believe this common vulnerability helped to create a shared sense of urgency among everyone who could influence the outcome of the pandemic, which was all of us.”
With an abundance of funding and focus on trying to stop the spread of COVID-19, researchers developed revolutionary advancements in their approaches to the disease. Although used under state-of-emergency conditions, these technologies will continue to transform the field of medical research, according to PubMed.
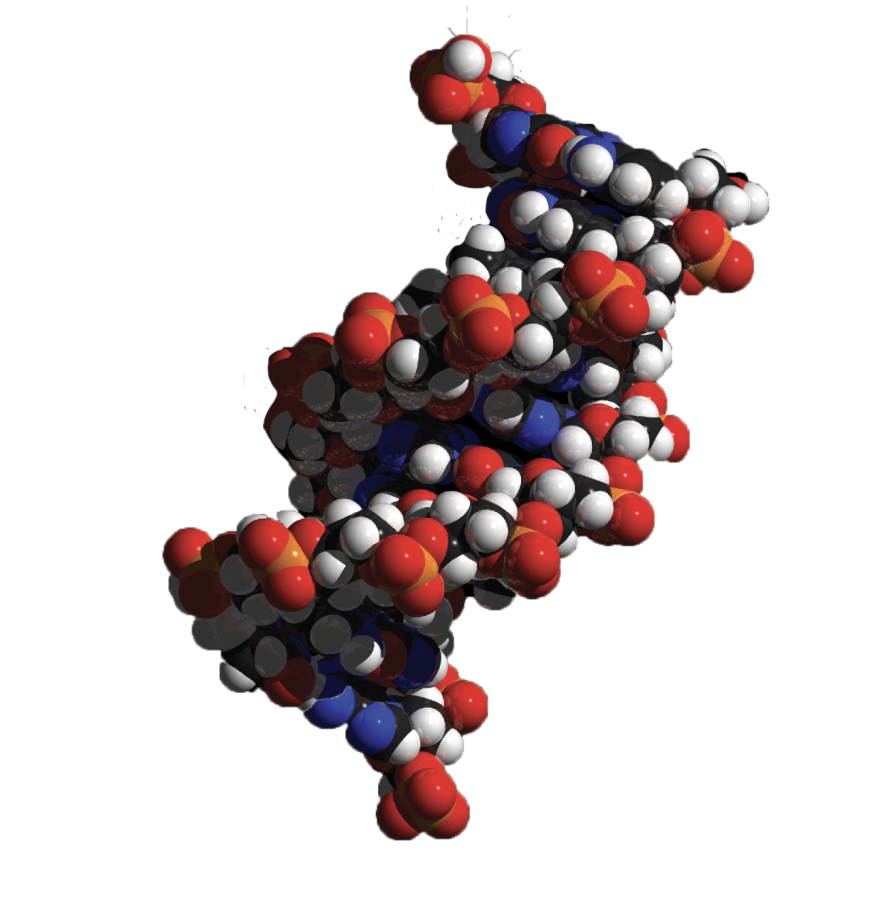
mRNA technology:
This revolutionary vaccine technology was used for the first time in manufacturing and distributing the Pfizer and Moderna COVID-19 vaccines. However, scientists had been working on the development of this type of vaccine for around 20 years, according to Johns Hopkins Bloomberg School of Public Health. This type of vaccine is different because rather than injecting a piece of the virus into the body, the mRNA inside the vaccine codes for the protein of COVID-19, so the body produces the protein and induces an immune response.
Scientists had been previously researching vaccines for related coronaviruses, SARS and MERS, which led to them to recognize the need for an mRNA vaccine as opposed to a conventional vaccine, according to Nature.
When COVID-19 struck, the mRNA technology had been refined by nanotechnology to allow it to properly function once injected into the body. Due to the $10 billion Operation Warp Speed vaccine program, researchers in biotech companies quickly completed preliminary testing to ensure the vaccine worked, according to Nature. The phases of vaccine trials were done simultaneously, allowing a vaccine to be approved and manufactured 11 months into the pandemic.
Other manufacturers are now looking into using this technology against other diseases such as the flu, according to Bloomberg School of Public Health. In addition, Moderna is researching its potential use in an HIV vaccine and scientists think vaccine development will be forever changed due to mRNA technology. However, the speed and efficiency to which the COVID-19 vaccine was distributed is attributed to the high number of infections and level of funding, according to Nature.
Clinical Trials
When the focus of the medical/research communities switched to the development of treatments and a vaccine for COVID-19, clinical trials were disrupted across other areas, according to PubMed. Clinical trial participants became unable to visit hospitals, while research staff were reassigned to work on COVID-19 treatments, according to Nature. Previously started large clinical trials were sometimes allowed to continue, especially those involving cancer treatment, but smaller, newer trials were often stopped. In addition, with the decrease in surgical procedures during the pandemic, researchers faced shortages in terms of human tissue, such as cancer tumors used in research.
The US Food and Drug Administration, however, adapted to the pandemic and altered the regulations for clinical trials. Participants could consent to a clinical trial virtually and get medicines delivered to their home. In addition, they could have more time between doctor visits, use online platforms to speak to doctors, and visit a local doctor rather than a research center for checkups. However, these policies did not work for all clinical trials in giving sufficient data, especially those that required medical imaging or short intervals between doctor visits, according to Nature.
Dr. Deborah Diercks, chair of Clinical Care and Research at UT Southwestern, conducted several clinical trials during COVID-19 that were specifically about diagnosis and treatment of the disease. One of her largest studies was serial testing for COVID-19 in first responders, investigating the rate of seroconversion and asymptomatic infections.
“COVID-19 research was essential, but as we transitioned into this research the major hurdle we had was gaining comfort from the research staff so we could start safely enrolling a large number of participants early on,” Diercks said. “Processes were streamlined, so we can ensure safe approval of studies in a more efficient manner.”
The lasting effects of COVID-19 on clinical trials include both positive and negative outcomes with doctors able to start up a clinical trial in less time, but a significant decrease in participants volunteering for trials.
“I think COVID-19 enhanced visibility of the need for collaboration across disciplines and the importance of being able to pivot to performing trials in different areas,” Diercks said.
Innovative Testing
COVID-19 brought new ways of testing to improve detection of disease. People could buy non-prescription infectious disease tests and perform them at home. Pharmacies, doctors’ offices and local clinics offered drive-thru testing. COVID-19 tests included technologies such as mass-spectrometry, artificial intelligence, and machine learning to identify if the virus was present in a sample, according to PubMed.
Dr. Jeffrey SoRelle and his lab members at UT Southwestern recently developed the testing technology “CoVarScan” that is able to identify which variant of COVID-19 is present, either Delta, Lambda, Mu, or Omicron. In June, SoRelle had tested 4,000 samples of infected COVID-19 patients and successfully reported the variants.
“Using this test, we can determine very quickly what variants are in the community and if a new variant is emerging,” SoRelle said in an interview to WFAA. “It also has implications for individual patients when we’re dealing with variants that respond differently to treatments.”
With the help of this new technology, North Texas public health leaders can track the spread of variants across the county. Doctors also can choose the right treatment for the way a specific variant might react.